Page 42 - Demo
P. 42
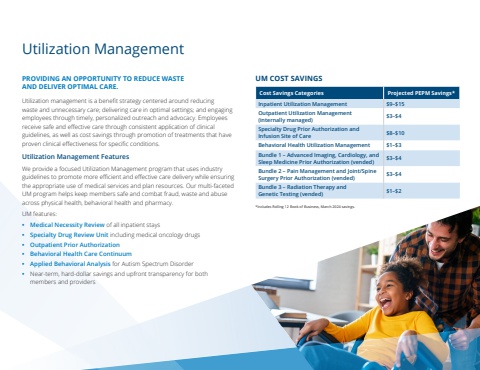
PROVIDING AN OPPORTUNITY TO REDUCE WASTE AND DELIVER OPTIMAL CARE.Utilization management is a benefit strategy centered around reducing waste and unnecessary care; delivering care in optimal settings; and engaging employees through timely, personalized outreach and advocacy. Employees receive safe and effective care through consistent application of clinical guidelines, as well as cost savings through promotion of treatments that have proven clinical effectiveness for specific conditions.Utilization Management Features We provide a focused Utilization Management program that uses industry guidelines to promote more efficient and effective care delivery while ensuring the appropriate use of medical services and plan resources. Our multi-faceted UM program helps keep members safe and combat fraud, waste and abuse across physical health, behavioral health and pharmacy. UM features:%u2022 Medical Necessity Review of all inpatient stays%u2022 Specialty Drug Review Unit including medical oncology drugs%u2022 Outpatient Prior Authorization%u2022 Behavioral Health Care Continuum%u2022 Applied Behavioral Analysis for Autism Spectrum Disorder%u2022 Near-term, hard-dollar savings and upfront transparency for both members and providersUtilization ManagementUM COST SAVINGSCost Savings Categories Projected PEPM Savings*Inpatient Utilization Management $9%u2013$15Outpatient Utilization Management (internally managed) $3%u2013$4Specialty Drug Prior Authorization and Infusion Site of Care $8%u2013$10Behavioral Health Utilization Management $1%u2013$3Bundle 1 %u2013 Advanced Imaging, Cardiology, and Sleep Medicine Prior Authorization (vended) $3%u2013$4Bundle 2 %u2013 Pain Management and Joint/Spine Surgery Prior Authorization (vended) $3%u2013$4Bundle 3 %u2013 Radiation Therapy and Genetic Testing (vended) $1%u2013$2*Includes Rolling 12 Book of Business, March 2024 savings.