Page 56 - Demo
P. 56
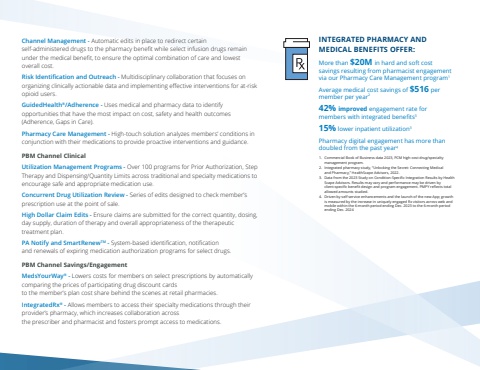
Channel Management - Automatic edits in place to redirect certain self-administered drugs to the pharmacy benefit while select infusion drugs remain under the medical benefit, to ensure the optimal combination of care and lowest overall cost.Risk Identification and Outreach - Multidisciplinary collaboration that focuses on organizing clinically actionable data and implementing effective interventions for at-risk opioid users.GuidedHealth%u00ae/Adherence - Uses medical and pharmacy data to identify opportunities that have the most impact on cost, safety and health outcomes (Adherence, Gaps in Care).Pharmacy Care Management - High-touch solution analyzes members%u2019 conditions in conjunction with their medications to provide proactive interventions and guidance.PBM Channel ClinicalUtilization Management Programs - Over 100 programs for Prior Authorization, Step Therapy and Dispensing/Quantity Limits across traditional and specialty medications to encourage safe and appropriate medication use.Concurrent Drug Utilization Review - Series of edits designed to check member%u2019s prescription use at the point of sale.High Dollar Claim Edits - Ensure claims are submitted for the correct quantity, dosing, day supply, duration of therapy and overall appropriateness of the therapeutic treatment plan.PA Notify and SmartRenewTM - System-based identification, notification and renewals of expiring medication authorization programs for select drugs.PBM Channel Savings/EngagementMedsYourWay%u00ae - Lowers costs for members on select prescriptions by automatically comparing the prices of participating drug discount cards to the member%u2019s plan cost share behind the scenes at retail pharmacies.IntegratedRx%u00ae - Allows members to access their specialty medications through their provider%u2019s pharmacy, which increases collaboration across the prescriber and pharmacist and fosters prompt access to medications.INTEGRATED PHARMACY AND MEDICAL BENEFITS OFFER:More than $20M in hard and soft cost savings resulting from pharmacist engagement via our Pharmacy Care Management program1Average medical cost savings of $516 per member per year242% improved engagement rate for members with integrated benefits315% lower inpatient utilization3Pharmacy digital engagement has more than doubled from the past year41. Commercial Book of Business data 2023, PCM high-cost drug/specialty management program. 2. Integrated pharmacy study, %u201cUnlocking the Secret: Connecting Medical and Pharmacy,%u201d HealthScape Advisors, 2022. 3. Data from the 2023 Study on Condition-Specific Integration Results by Health Scape Advisors. Results may vary and performance may be driven by client-specific benefit design and program engagement. PMPY reflects total allowed amounts studied.4. Driven by self service enhancements and the launch of the new App; growth is measured by the increase in uniquely engaged Rx visitors across web and mobile within the 6-month period ending Dec. 2023 to the 6-month period ending Dec. 2024