March 2022
Any Provider Accepting Medicare Can See Flex Plan Members
In November, we told you about the new Blue Cross Medicare Advantage Flex (PPO)SM plan. As of Jan. 1, 2022, Flex plan members can see any provider in the U.S. who accepts Medicare. Here are questions and answers about the plan and how it may affect your payments.
How do I recognize Flex plan members?
You can identify Flex plan members by their Blue Cross and Blue Shield of Illinois (BCBSIL) member ID card. Look for the Flex plan name on the front:
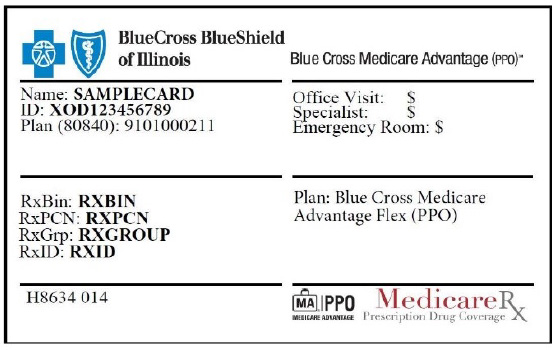
Members may give you information they received with their Flex plan welcome kit that includes a toll-free number for claims questions: 877-774-8592. Calls are answered between 8 a.m. and 8 p.m. daily.
Is this a Medicare Supplement plan?
No. This plan is a Medicare Advantage Prescription Drug (MAPD) plan (PPO). It provides access to any provider who accepts Medicare and agrees to bill BCBSIL. It includes medical coverage and prescription drug coverage. All claims are paid by BCBSIL.
How do Medicare Parts A and B work with the Flex plan?
The Flex plan is a Medicare Advantage PPO plan. It covers the same benefits as Parts A and B as well as additional benefits per plan. Members are required to pay a premium for this plan.
Who can see Flex plan members?
- Any provider who accepts Medicare assignments and bills BCBSIL can see Flex plan members.
- The Flex plan is an open access plan. Members may access providers contracted with any Blue Cross and Blue Shield (BCBS) plan or non-contracted providers willing to bill BCBSIL.
- Medicare providers don’t need to have a Medicare Advantage contract with BCBSIL to see a member under the Flex plan.
- Providers who don’t have contracts with Medicare may not accept Flex plan members.
How do I get reimbursed if my patients are in this plan?
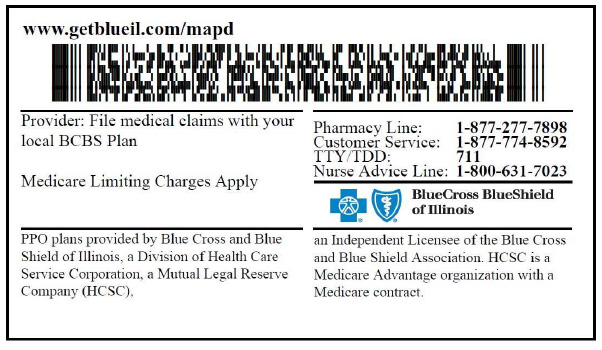
- Follow the billing instructions on the member’s ID card and file claims with BCBSIL.
- If you are a Medicare Advantage-contracted provider with any BCBS plan, you will be paid at your contracted rate. You are required to follow utilization management review requirements and guidelines. Learn more about prior authorization below.
- If you are not a Medicare Advantage-contracted provider with BCBS, you will receive the Medicare allowed amount for covered services. You may not balance bill the member for any difference in your charge and the allowed amount. You do not need to follow prior authorization guidelines.
- If you have questions about submitting claims or receiving payment, call 877-774-8592 between 8 a.m. and 8 p.m. daily.
What if I treat a member outside their plan service area?
Follow the billing instructions on the member’s ID card and bill BCBSIL.
Are prior authorizations required for the Flex plan?
Some services require prior authorization. Learn about utilization management and view our prior authorization summary and code lists on our website. Always check eligibility and benefits first via Availity Essentials® or your preferred web vendor prior to rendering care to our members. This step will confirm prior authorization requirements and utilization management vendors, if applicable. If you have questions specific to Flex plan members, call 877-774-8592.
For non-participating providers: You aren’t required to follow utilization management guidelines. However, you may request a review to confirm medical necessity, as is typical for other MAPD PPO plans.
Can Medicare recipients with pre-existing health conditions enroll in this plan?
Yes. Like all Medicare Advantage plans offered through BCBSIL, there are no pre-existing exclusions with the Flex plan.
Checking eligibility and/or benefit information and/or obtaining prior authorization or pre-notification is not a guarantee of payment. Benefits will be determined once a claim is received and will be based upon, among other things, the member’s eligibility and the terms of the member’s certificate of coverage, including, but not limited to, exclusions and limitations applicable on the date services were rendered. If you have any questions, call the number on the member's ID card.
Availity is a trademark of Availity, LLC, a separate company that operates a health information network to provide electronic information exchange services to medical professionals. Availity provides administrative services to BCBSIL. BCBSIL makes no endorsement, representations or warranties regarding any products or services provided by third party vendors such as Availity.
