November 2021
Submitting Electronic Replacement or Corrected Claims
The Blue Cross and Blue Shield of Illinois (BCBSIL) claim system recognizes claim submission types on electronic claims by the frequency code submitted. The ANSI X12 837 claim format allows you to submit changes to claims that were not included on the original adjudication.
Claim Frequency Codes
The 837 Implementation Guides refer to the National Uniform Billing Data Element Specifications Loop 2300 CLM05-3 for explanation and usage. In the 837 formats, the codes are called “claim frequency codes.” Using the appropriate code, you can indicate that the claim is an adjustment of a previously submitted finalized claim.
Use the below frequency codes for claims that were previously adjudicated:
Claim Frequency Codes |
|||
Code |
Description |
Filing Guidelines |
Action |
5 - Late Charge(s) (Institutional Providers Only) |
Use to submit additional charges for the same date(s) of service as a previous claim. |
File electronically, as usual. Include only the additional late charges that were not included on the original claim. |
BCBSIL will add the late charges to the previously processed claim. |
7 - Replacement of Prior Claim |
Use to replace an entire claim (all but identity information). |
File electronically, as usual. File the claim in its entirety, including all services for which you are requesting reconsideration. |
BCBSIL will adjust the original claim. The corrections submitted represent a complete replacement of the previously processed claim. |
8 - Void/Cancel of Prior Claim |
Use to entirely eliminate a previously submitted claim for a specific provider, patient, insured and "statement covers period." |
File electronically, as usual. Include all charges that were on the original claim. |
BCBSIL will void the original claim from records based on request. |
Submitting Electronic Replacement Claims
When submitting claims noted with claim frequency code 7 or 8, the original BCBSIL claim number (also referred to as the Document Control Number or DCN) must be submitted in Loop 2300 REF02 – Payer Claim Control Number with qualifier F8 in REF01. The DCN can be obtained from the 835 Electronic Remittance Advice (ERA) or Electronic Payment Summary (EPS).* Without the original BCBSIL DCN, adjustment requests will generate a compliance error and the claim will reject. BCBSIL only accepts claim frequency code 7 to replace a prior claim or claim frequency code 8 to void a prior claim.
Specific information and examples for Professional and Institutional providers are included below.
Professional Providers:
Claim corrections submitted without the appropriate frequency code will deny and the original BCBSIL claim number will not be adjusted. For more information on submitting electronic replacement claims, refer to the table and example below.
Code |
Action |
7 - Replacement of Prior Claim |
BCBSIL will adjust the original claim. The corrections submitted represent a complete replacement of the previously processed claim. |
8 - Void/Cancel of Prior Claim |
BCBSIL will void the original claim from records based on request. |
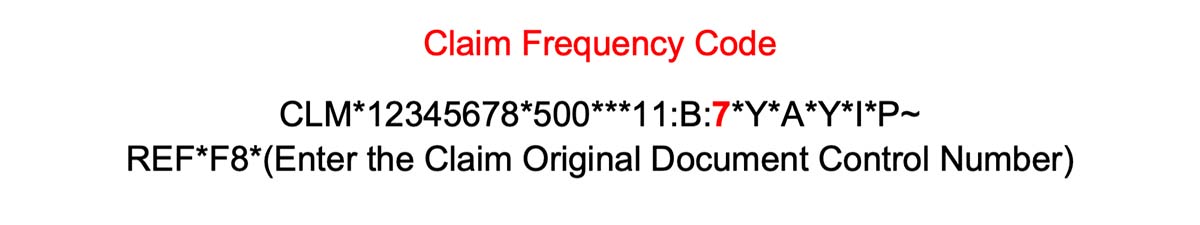
An example of the ANSI 837 CLM segment containing the claim frequency code 7, along with the required REF segment and Qualifier in Loop ID 2300 - Claim Information, is provided below.
Institutional Providers:
Claim corrections submitted without the appropriate frequency code will deny as a duplicate and the original BCBSIL claim number will not be adjusted. For more information on submitting electronic replacement claims, refer to the table and example below.
Code |
Action |
5 - Late Charge(s) |
BCBSIL will add the late charges to the original claim processed claim. |
7 - Replacement of Prior Claim |
BCBSIL will adjust the original claim. The corrections submitted represent a complete replacement of the previously processed claim. This code is not intended to be used in lieu of late charges. |
8 - Void/Cancel of Prior Claim |
BCBSIL will void the original claim from records based on request. |
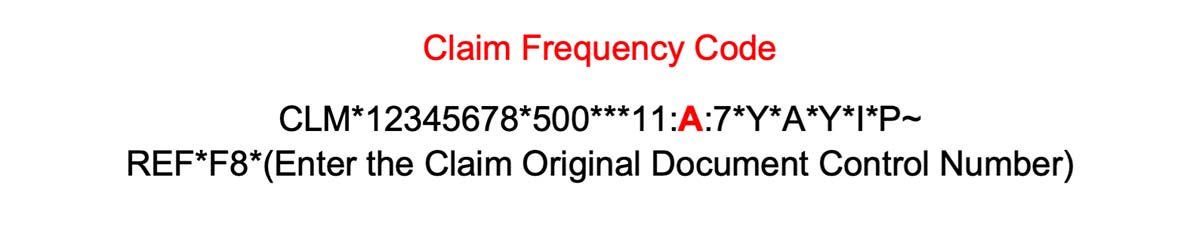
When submitting corrected institutional claims, take note of CLM05-2, the Facility Code Qualifier. In this instance, the CLM05-2 field would require a value of “A” indicating an institutional claim – along with the appropriate frequency code (7) as illustrated in the example below.
Note: If a charge was left off the original claim, submit the additional charge with all of the previous charges as a replacement claim using frequency code 7. All charges for the same date of service should be filed on a single claim.
Frequency Code 5, Late Charge(s) applies strictly to institutional claims.
For more information on professional electronic replacement claims, visit the Claim Submission section of our Provider website.
*EPS files are not available for Blue Cross Community Health PlansSM (BCCHPSM), Blue Cross Community MMAI (Medicare-Medicaid Plan)SM, Blue Cross Medicare Advantage (HMO)SM and Blue Cross Medicare Advantage (PPO)SM claims.
