February 2021
Medicaid Claim Filing Reminder: Don’t Enter a P.O. Box in Field 33
Our Blue Cross Community Health PlansSM (BCCHPSM) and Blue Cross Community MMAI (Medicare-Medicaid Plan)SM products are aligned with Illinois Department of Healthcare and Family Services (HFS), Health Insurance Portability and Accountability Act (HIPPA) 5010 standards, and National Uniform Claim Committee (NUCC) billing requirements specific to filing professional claims.
Recently, we’ve received several questions from providers about a billing error in field 33 that’s causing claim rejections. Here are some quick reminders that may be helpful.
Electronic Claims
For professional electronic claim submissions (837P transactions), the provider’s billing address must be an actual street address in the following location: Loop ID 2010AA. Providers may use a P.O. Box, but only in the Pay-To address location on electronic claims.
When conducting electronic data interchange (EDI) transactions, health care providers, billing agents and clearinghouses must follow HIPAA standards. It’s your responsibility to obtain and follow EDI transaction standards specified within the current ANSI X12 837 – ANSI 5010 Technical Reports Type 3 (TR3). For details, refer to the X12 website.
Paper Claims
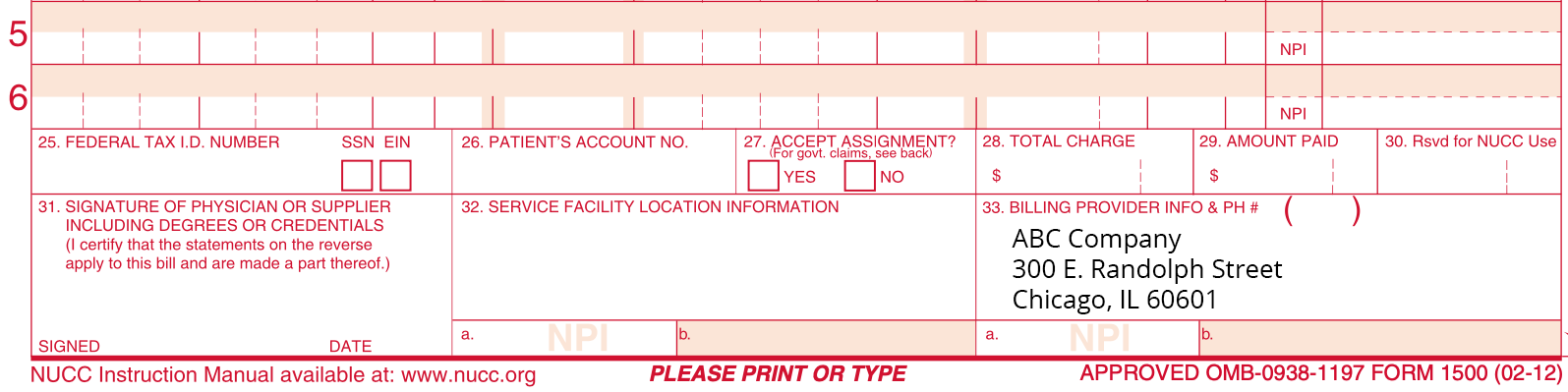
A physical address is required for the provider’s billing location in field 33 of the paper CMS-1500 claim form. Any paper claims submitted with a P.O. Box as the provider’s billing address in field 33, will be rejected. See example below. For more information on paper claim filing guidelines, refer to the NUCC Reference Instruction Manual.
Questions? Call Customer Service at 877-860-2837 or contact your assigned Provider Network Consultant (PNC).
References to third party sources or organizations are not a representation, warranty or endorsement of such organizations. Any questions regarding those organizations should be addressed to them directly.
