April 2021
Medicaid Billing Reminders for Home and Community Based Services (HCBS) Waiver Providers
This article applies to HCBS providers – Illinois Department of Healthcare and Family Services (HFS) types 90, 92, 93 and 98 – who submit claims to Blue Cross and Blue Shield of Illinois (BCBSIL) for our Blue Cross Community Health PlansSM (BCCHPSM) and Blue Cross Community MMAI (Medicare-Medicaid Plan)SM members.
BCBSIL has aligned its claim coding with HFS managed care billing and guidelines for HCBS waiver providers regarding Medicaid claims for Managed Care Organizations (MCOs). HCBS providers should also refer to the Illinois Association of Medicaid Health Plans (IAMHP) Comprehensive Billing Manual, available on the IAMHP website.
When billing HCBS services, HCBS provider types should only use their HFS Legacy Provider Numbers (Medicaid IDs) – they should not use their National Provider Identifiers (NPIs) on Medicaid claims. On BCCHP and MMAI member claims, the HFS Legacy Provider Number (Medicaid ID) must match the Illinois Medicaid Program Advanced Cloud Technology (IMPACT) Legacy Provider Number (Medicaid ID). BCBSIL won’t be able to process the claim if the HFS Legacy Provider Number (Medicaid ID) used doesn’t match the corresponding IMPACT Legacy Provider Number (Medicaid ID) and IMPACT-registered categories of service, specialties, etc. The provider’s HFS Legacy Provider Number (Medicaid ID) must match the IMPACT-registered provider type that corresponds with the member’s waiver type.
Illinois Medicaid HCBS Billing Waiver – Electronic Claim Submission
Atypical providers rendering HCBS for our BCCHP and MMAI members may submit electronic professional claims (837P transactions) to BCBSIL. These claims may be submitted through your practice management system, the Availity® Provider Portal, or another preferred web vendor using Payer ID MCDIL.
To accurately submit these claims to BCBSIL using Availity’s Electronic Professional Claim Submission tool, a valid Legacy Provider Number (Medicaid ID) is required in the Payer Assigned ID field (2010BB-REF*G2). For the Payer Assigned ID field to appear on the Availity 837P submission, your Availity Administrator must first add your information to enable Availity’s Express Entry function, as follows:
How to Set-up Availity’s Express Entry (Instructions for Availity Administrators)
- Log in to Availity
- Select “My Providers” from the navigation menu
- Select “Express Entry”
- Select “Add Provider” and click the link for “This provider is not required to have an NPI”
- Enter the Atypical Provider Information, including the Tax ID number
- Select “Save Provider”
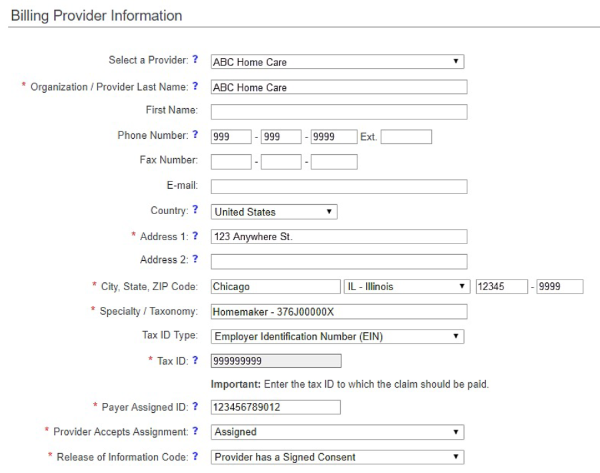
After the Express Entry set-up is completed, you may use the “Select a Provider” drop-down listing in the Billing Provider Information section on the Availity 837P submission tool. Your associated provider data will populate, and the Payer Assigned ID field will appear to enter the 12-character Medicaid ID.
If you need training or help with electronic claim submission, email our Provider Education Consultants.
What to Do if You Have Multiple Registrations with HFS
If you have multiple registrations with HFS for provider types outside of the HCBS service realm, only include your NPI on claims for non-HCBS services. For example, if you’re registered as an HFS Home Health provider type (050) and also registered as an HCBS provider (090), and you’re billing for Home Health services, you must submit an electronic institutional provider claim (837I transaction) using your NPI in the 2010AA Billing Loop. When billing as HCBS with HFS provider type 090, you must submit an electronic professional claim (837P) using your Medicaid ID without an NPI. Refer to the Home Health Care section of the Comprehensive Billing Manual on the IAMHP website for billing rules to MCOs.
Personal Assistants and Individual Providers
BCBSIL works with our members to develop individualized care plans that may include personal assistants. We will provide care coordination and oversight of the services being provided to our BCCHP and MMAI members. Personal Assistants (PAs) and Individual Providers (IPs) that are not working through an agency are required to enroll in IMPACT. When seeking reimbursement, PAs and IPs may not submit claims directly to the MCOs. They are required to log their time using the electronic visit verification system so that payment can be issued by the State of Illinois.
Electronic Data Interchange (EDI) – Claim Rejection Update
HCBS providers should take note of a new EDI claim rejection that’s based on validating the presence of the provider’s HFS Medicaid ID on the claim. If the HFS Medicaid ID is missing, this is the rejection that will be returned in the 277CA Claims Acknowledgement:
STC Segment |
Data Value |
STC01-01 |
A3 |
| STC01-02 | 562 |
| STC01-03 | 85 |
| STC12 | Waiver claims should not be submitted with an NPI |
For more information, refer to the appropriate Provider Manual. If you have questions, email your Provider Network Consultant (PNC) or call 855-653-8126.
Availity is a trademark of Availity, LLC, a separate company that operates a health information network to provide electronic information exchange services to medical professionals. Availity provides administrative services to BCBSIL. BCBSIL makes no endorsement, representations or warranties regarding any products or services provided by third party vendors such as Availity. If you have any questions about the products or services provided by such vendors, you should contact the vendor(s) directly.
